In the eleventh installment of the Immunology 101 Series, Aimee will explain the basics of the infectious disease mumps and the science behind the vaccines available for mumps.
If you have been paying attention to the news over the past several months, you have likely heard from multiple sources that mumps has recently made a comeback in the United States. In Colorado, there have already been close to 50 cases reported in 2017, primarily from the Denver metro area, compared to only 17 total cases for the entire year of 2016. Because mumps is thought to be a disease of the past and most of us haven’t been affected by this infectious disease firsthand, many people have questions surrounding the disease itself and the vaccine that was created to prevent it. As always, I will use my background as a scientist to help you understand the facts related to mumps and the vaccine that was created to protect us. Let’s get started….
What is mumps?
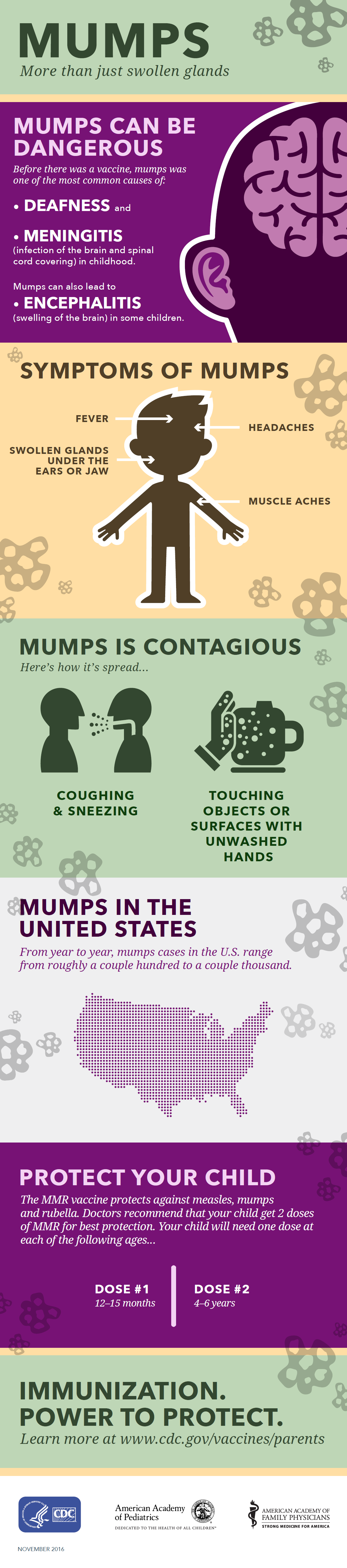
Mumps is a contagious disease caused by the mumps virus that most commonly begins with fever followed by inflammation of the major salivary glands, typically 2-3 weeks after the initial infection. When the major salivary glands, also called the parotids, are infected by the mumps virus they become inflamed and expand in size to cause the symptom most associated with mumps – big, puffy ‘chipmunk’ cheeks – which is called parotitis. For a quick review, inflammation is a protective response produced by the immune system, the body’s military defense system. Inflammation is actually the recruitment and accumulation of cells of the immune system, also called white blood cells, to the area of infection. You can think of inflammation as the immune military reporting for active duty to the site of infection to fight and destroy the offending pathogen.
Is the mumps virus contagious?
Yes! Mumps outbreaks can occur at any time of the year as a result of direct contact. The mumps virus replicates, or produces more virus, in the respiratory tract and is spread through direct contact with saliva or respiratory secretions (through coughing, sneezing, kissing, sharing utensils or drinking soda out of the same can, etc.). If other people breathe the contaminated air (e.g. think elevator or crowded university classroom) or touch an infected surface (e.g. think doorknob or vending machine), then touch their eyes, noses, or mouths, they can become infected. The best way to prevent the spread of the virus is for the people infected with mumps to avoid contact with others from the time of diagnosis until at least 5 days after the onset of salivary gland inflammation or parotitis.
Is mumps a serious disease?
The short answer is yes. Mumps, like any infectious disease, can be serious. In most cases, mumps infection causes people to have a fever, feel tired and achy, and have swollen salivary glands. Sometimes the swollen salivary glands cause severe jaw pain that makes eating difficult. Most people infected with mumps recover completely within a few weeks. However, in rare cases mumps can cause inflammation of the brain (encephalitis) or the protective membranes covering the spinal cord and brain (meningitis), which can lead to permanent injury or death. Other serious, but rare, complications associated with mumps infection include hearing loss and, in some adolescent boys and men, pain or swelling of the testicles (orchitis), or in some adolescent girls and women, infection and swelling of the ovaries (oophoritis), or infection and swelling of the pancreas (pancreatitis).
Is the vaccine against mumps safe and effective?
As a scientist who has read the literature, I know that the vaccines available for mumps are safe and effective. I also understand that the risk from the vaccine is minimal compared to the danger of becoming sick from the mumps. The only mumps vaccine available in the United States is a live, attenuated (weakened and non-disease causing) version of the virus. It is available as a combination with measles and rubella vaccines, called the MMR vaccine, or with an additional varicella (aka chicken pox) vaccine, called the MMRV vaccine. Live-attenuated vaccines are highly effective. Immunologists love live-attenuated vaccines as they most closely resemble a natural infection and produce a vigorous immune response that most often lasts a lifetime due to the amazing ‘army’ of immune cells produced during the immune response to the vaccine.
To ensure your immune system is equipped with an amazing immune ‘army’ ready to fight the mumps virus upon infection, 2 doses of the vaccine are recommended for children (first dose at age 12-15 months and second dose at age 4-6 years before school entry) and adults at high risk for exposure and transmission. Adults at high risk would include international travelers (keep in mind that not everyone around the globe has access to this vaccine), people who work in healthcare, and people in crowded environments such as those attending university or living in dorms. It is important to understand that in the United States, widespread use of the mumps vaccine since it was first introduced has led to a greater than 99% reduction in mumps cases compared to years preceding the vaccine.
Why are we seeing more cases of mumps?
In 2006 and 2016 mumps epidemics, primarily in teenagers and young adults, occurred in different regions of the country. Surprisingly, many, but not all, of the people that became ill with the mumps during these epidemics had received the recommended 2 doses of the vaccine. After investigating the current strains of the mumps in circulation and the ability of vaccinated individuals to respond to these strains, scientists concluded that the mumps vaccine is still accurate (i.e. targeting the proper strain). So, if the vaccine still targets the appropriate strain, what is the problem? It turns out that immunity to the mumps virus likely fades over time. Protective immunity may fade just enough that vaccinated individuals, such as the older teenagers and young adults swept up in the recent epidemics who last had the second dose of the mumps vaccine 10 or more years ago, are susceptible to infection. Interestingly, the more serious complications of mumps infection, such as encephalitis, hearing loss and pancreatitis, have not been observed in individuals previously vaccinated. This suggests that the vaccine is still protective, in the sense that it prevents the more serious complications, even after immunity has faded.
Take home message
Do not hesitate to immunize your children with the MMR (or MMRV) vaccine to protect them, your family, and the people in your community. The MMR (and MMRV) vaccine is safe and effective and will protect you and your loved ones from a potentially serious infectious disease.
More resources:
- Mumps Information – Centers for Disease Control (CDC)
- Mumps Vaccination – CDC
- A Look at Each Vaccine: Measles, Mumps and Rubella Vaccines – Children’s Hospital of Philadelphia (CHOP) Vaccine Education Center
- ‘Why Are We Still Getting Mumps,’ by Paul Offit, MD – The Daily Beast
- Mumps – Immunize for Good