This post was originally published on April 4, 2013 and updated on March 17, 2020.
In the third installment of the Immunology 101 Series, Aimee explains the process of vaccine development. Vaccines undergo rigorous testing and must be proven extremely safe and effective before they are available for use in the general public.
As you may know from reading the first Immunology 101 Series post, vaccines train our immune systems to recognize and respond quickly to infection to keep us healthy. Reading the second Immunology 101 Series post, you learned that there are several different forms of vaccines, each created to produce the most effective vaccine possible based on the unique properties of each type of pathogen. In this post you will learn about the process of vaccine development. The process is lengthy and rigorous, just as it should be to prove that the end product is safe and effective!
How are vaccines actually made?
As you might imagine, long before vaccines are actually produced, researchers spend several years studying how the pathogen causes disease. They also spend lots of time determining other helpful factors related to vaccine design, such as what type of vaccine would be best (i.e. live, attenuated or inactivated or conjugate, etc.) and how many doses are needed to produce a vigorous and protective immune response. After this essential information has been worked out there are several phases of testing that need to be performed to ensure safety and efficacy before the vaccine can be used.
Phase I • The Phase I studies are designed to determine if the vaccine is safe and effective (if it induces an immune response*) in the participants of the study. The type of people that typically participate in Phase I studies are at a low risk for infection and consist primarily of healthy individuals.
* The induction of an immune response, or activation of the cells of the immune system, is absolutely essential. It is important to understand that not every person responds the same way to each pathogen. Vaccine biologists, the scientists that create vaccines, need to determine which formulation of each pathogen induces an immune response in the most people.
Phase II • The Phase II studies only occur if the vaccine has passed Phase I. The questions asked within this second phase are similar (such as, is the vaccine safe and effective?) but are tested in a much larger group of study participants (i.e. several hundred) that more closely represent the people that would use the vaccine if and when it becomes available.
Phase III • The Phase III studies only occur if the vaccine has passed Phase II. Again, the questions asked within this third phase are similar to the other phases (such as, is the vaccine safe and effective?) but performed in thousands of people and studied for much longer periods of time, often for many years. Additionally, several different types of people are included to ensure that the vaccine is safe and effective in a diverse group of people. The Phase III studies routinely include participants from different geographic areas with varied backgrounds and ways of life.
Review of Phases I, II and III by several official agencies
After the first three phases are complete, the results will be reviewed by the United States Food and Drug Administration (FDA). The FDA will extensively review the data and results from Phase I, II, and III to ensure that the vaccine has demonstrated that it is both safe and effective. At this point many other scientific and medical experts are needed to confirm the findings and make recommendations on the use of the vaccine. The first of these additional experts are from the Advisory Committee on Immunization Practices (ACIP), which is a specialized division of the Centers for Disease Control and Prevention (CDC) that develops recommendations for the use of vaccines to control diseases in the U.S. Medical doctors from the American Academy of Pediatrics (AAP) and the American Academy of Family Physicians (AAFP) are also involved and, together with the ACIP, make final decisions for the use of the vaccine. It’s important to understand that the science is collaborative and relies on the combination of many experts to ensure the data is accurate and the science is reliable.
Post-Licensing • The safety and efficacy of each and every vaccine is so important that vaccines are continually monitored after licensure and distribution to the general population to ensure that long-term efficacy, as well as any additional rare side effects occur, are recorded.
Monitoring within this post-licensing phase includes oversight by the CDC of every health department in the country to track disease occurrence, along with the Vaccine Safety Datalink (VSD) and the Vaccine Adverse Events Reporting System (VAERS). The Vaccine Safety Datalink, or VSD, is a collaborative effort between the CDC’s Immunization Safety Office and several managed care organizations (MCOs) across the country and was established to monitor immunization safety and further record any rare and/or serious events following immunization. The Vaccine Adverse Events Reporting System, or VAERS, is a national reporting system created by the FDA and CDC to accept 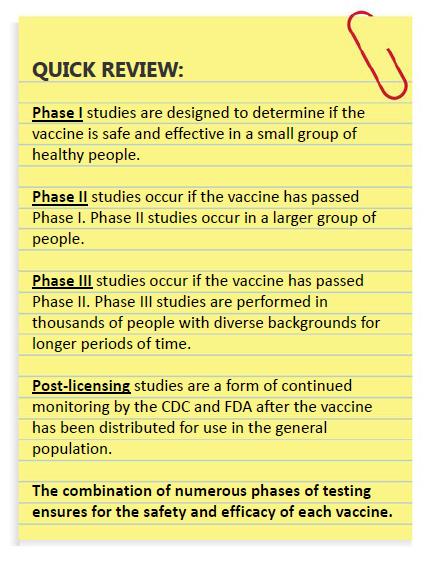
It is also important to understand that protection from vaccines is not absolute. Individual immune systems can react differently to vaccines, which may account for the rare occasions when people are not protected by immunization or when they experience side effects. Just like every individual is unique, so are their immune systems and the way in which they might respond to vaccines. However, due to safety and efficacy trials, we know that the majority of people who are vaccinated will be safety and effectively protected from disease.
Summary
Scientists, government agencies and healthcare providers do their best to provide safe and effective vaccines. Each vaccine created and distributed in the United States undergoes a combination of several phases of testing over many years to protect the general public from multiple harmful infectious diseases.
Sources:
Varricchio F, Iskander J, Destefano F, Ball R, Pless R, Braun MM, Chen RT. Understanding vaccine safety information from the Vaccine Adverse Event Reporting System. Pediatric Infectious Disease Journal 2004;23(4):287–294.
Zhou W, Pool V, Iskander JK, English-Bullard R, Ball R, Wise RP, Haber P, Pless RP, Mootrey G, Ellenberg SS, Braun MM, Chen RT. Surveillance for safety after immunization: Vaccine Adverse Event Reporting System (VAERS)—United States, 1991–2001. MMWR 2003;52(1):1–24.
Chen RT, Rastogi SC, Mullen JR, Hayes SW, Cochi SL, Donlon JA, Wassilak SG. The Vaccine Adverse Event Reporting System (VAERS). Vaccine 1994;12(6):542–550.
